Uncovering the Complex Pathways of Alzheimer’s Disease
Finding a way to slow or even stop Alzheimer’s disease is one of the most difficult challenges facing medicine today. Many research and clinical trials have led to promising results over the years, while others have produced disappointing findings. But what if there were a way to get more out of these trials—even the ones with less-than-promising results? What if there were a better way to determine if a drug is hitting its intended target?
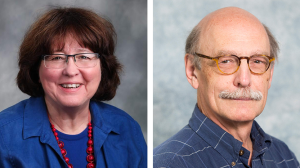
The work of two Duke collaborators, Carol Colton, PhD, and W. Kirby Gottschalk, PhD, may lead to answers to these pressing questions and offer a more promising outlook for people suffering from Alzheimer’s disease.
With funding from philanthropy, Colton and Gottschalk have teamed up to understand the effects of the changes that occur in metabolic pathways in patients with Alzheimer’s disease. Instead of looking at one cell at a time, they are finding ways to look at multiple networks. The researchers say that their approach is key to discovering how metabolic changes lead to Alzheimer’s disease.
“Our work points to a specific immune-regulated metabolic pathway that is disordered in Alzheimer’s disease,” says Colton, a professor in the Department of Neurology. This pathway has an impact on not only neurons but also on other cells in the brain.
“AD does not involve only a single cell—it’s not just a neuron or a macrophage,” she says. “It’s a combination of cells, all trying to survive together. Essentially you have to look at Alzheimer’s disease as an immune-based ‘brain’ disease. Alzheimer’s disease represents a complex multicellular problem, and you can’t cure it by singling one cell type out and saying, ‘We’re going to fix you.’”
Therefore, to understand how metabolic changes occur and why they lead to Alzheimer’s disease, it is important to determine the ramifications of the metabolic changes throughout the rest of the network.
In their research, funded through the Holland-Trice Scholars Program, Colton and Gottschalk are studying the metabolic changes in real time using mice whose immune systems have been engineered to look like those in humans with Alzheimer’s disease.
“A while ago, Dr. Colton began to draw attention to the fact that there are immune cells in the brain called microglia, and that these microglia are disturbed in Alzheimer’s disease,” says Gottschalk, assistant professor of neurology. “And this is where the focus really should lie.”
Although we do not understand the underlying reason why microglia are disrupted in Alzheimer’s disease, when microglia are “turned on” during an immune response, they begin to consume metabolites and amino acids such as arginine. Their actions cause microglia to take away needed nutrients from nearby cells including neurons. The result appears to be redirection of critical metabolic pathways to generate other compounds that contribute to the disease process. Without the nutrients they need, cells including neurons aren’t able to function normally. This may occur in Alzheimer’s disease.
In their research, Gottschalk and Colton are treating mouse models of Alzheimer’s disease with arginine isotopes that are heavier than normal but are also nontoxic. They then use mass spectrometry to trace the pathway of the heavy-labeled arginine and other metabolites such as polyamines throughout the brain and in various fluids (blood, urine) and tissues in the rest of the body.
“It gives us the ability to understand which pathway is changed in AD, and which metabolic direction may be important for treatment,” Colton says. “And it enables us to see if a treatment is, in fact, therapeutic.”
Though the research has been done in mice, Gottschalk says it could be replicated in humans. The isotopes used in their study are not radioactive; therefore, they are safe to use in humans and have already been used previously in human trials. Also, collecting small amounts of cerebral spinal fluid could be used to follow the path of the heavy-labeled arginine and polyamines over the course of the disease.
“By injecting a small amount of heavy-labeled arginine into a human, we could sample the cerebral spinal fluid, measure the isotope level, and use the data as a surrogate measure of what’s going on in the brain,”
W. Kirby Gottschalk, PhD
Colton and Gottschalk say the next step is clinical trials in humans.
Ultimately their research could allow researchers to measure the distribution of the isotope in biological fluids such as cerebral spinal fluid, plasma, or urine, giving them and patients participating in clinical trials a better idea of whether a tested drug is hitting its intended target. The research could also help in developing new drugs that have not been previously considered for use in Alzheimer’s disease.
Colton says the clinical trial participants “want to have an idea that the drugs they are testing will work on Alzheimer’s disease and bring hope to either themselves or to other people. But you need a system that has the ability to cleanly and clearly say that the drug you are testing is working or not.”
Gottschalk adds, “A lot of drug trials, including those involved with AD, are conducted throughout the country each year, and either they work or they don’t work. If they do not work, you are unfortunately left many times with not knowing exactly why it didn’t work. With this isotope pathway tracing mechanism, we’ll know if altering a specific pathway is important to treatment or not.”
Thanks to the support of donors, who allowed them to conduct this work, Colton and Gottschalk say they have gone on to apply for two National Institute on Aging grants. They also have now presented preliminary results at various Alzheimer’s disease-based meetings.