Patient’s Gift Launches Melanoma Survivorship Program
Prior to 2011, the life expectancy of an individual diagnosed with metastatic melanoma was generally measured in months. There were no good treatment options. Among patients diagnosed with stage 4 melanoma, 50% developed metastasis to the brain, and only 5% were still alive five years after diagnosis.
Today the situation is dramatically different. Thanks largely to the ongoing development of effective immunotherapies, many patients diagnosed with advanced melanoma are not only still alive at the five- or ten-year mark, but have yet to have a recurrence.
The phenomenal success of immunotherapy means there is a new population of cancer survivors with unique needs. Duke has several hundred patients who have completed treatment for advanced melanoma. They are considered cancer-free, but also need post-treatment care and monitoring.
To help these patients, an anonymous donor who received his melanoma care at Duke has given $1 million to fund a survivorship program.
“My experience brought home to me that this is a very important part of Duke and an area worthy of support because the investment in research is paying dividends, not just for me, but for hundreds of thousands of people around the world,” said the donor. “The survivorship program is going to help Duke treat more people, and provide that treatment more effectively and efficiently.”
Coordinating, Personalized Care
Immunotherapy has proven to be a durable treatment that works by taking the brakes off the immune system so that it can more effectively attack cancer cells. But because immunotherapies are relatively new, physicians don’t fully understand their implications for long-term health. They also don’t know if immunotherapy “cures” melanoma or if recurrences will happen, albeit at longer intervals.
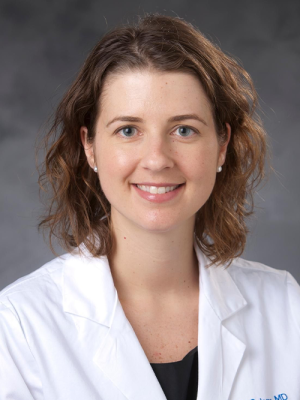
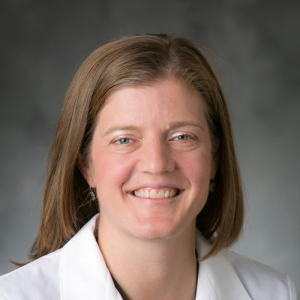
The survivorship program will be co-led by medical oncologist April Salama, MD, and surgical oncologist Georgia Beasley, MD, MHS, who also direct Duke Cancer Institute’s melanoma and advanced skin cancers disease group.
“Anywhere from about 15 to 50% of patients, depending on which treatment regimen they receive, will have a serious side effect, and for a small subset of those patients the side effects, especially those that impact the endocrine system, will be permanent,” said Beasley. “These patients require care coordination across multiple specialties.”
Side effects range from issues that typically resolve over time, like skin or bowel inflammation and brain fog, to ones that are permanent, including hypothyroidism and type 1 diabetes. The program will add staff to coordinate care for these patients across disciplines, freeing up the oncology team to see patients who are newly diagnosed and in need of therapy.
“As patients progress to different levels of care, they don't need to see us as frequently, but they still need to be connected to care,” said Salama. “This program will bring the care closer to the patient, even those that live hours away from Duke, for whom continued care can become a huge burden. Ultimately, we want to ensure people will continue with their care, and this program will give us the resources to provide consistent, high-quality care.”
Improving Care Globally
The program will also focus on developing best practices to improve care for immunotherapy patients everywhere.
“There are a lot of unknowns, given how new this population is,” said Beasley. “Part of the program will focus on research to inform best practices, to understand what is the right frequency and which types of monitoring are most informative. We want to understand patients who respond really well to immunotherapy. Can we identify what contributed to these patients’ exceptional response and use it to help others? We also want to figure out easier, less invasive ways to screen patients.”
A recent advance that shows promise as an early screening tool is a blood test that can detect tumor DNA well before the melanoma can be detected by other means.
“It is not often that a whole new class of survivors is created, but with advances in technology and our understanding of cancer biology we are beginning to see this happen more and more,” said Peter Allen, MD, chief of the Division of Surgical Oncology. “This gift will enable us to better serve all our patients including those newly diagnosed, in treatment, and post treatment, and just as importantly, to improve the care every melanoma survivor receives. We are incredibly grateful.”
For the donor it was important to thank his team for their exemplary care.
“Everyone — the doctors and staff — was extremely competent and engaging. They made time for all my questions,” he said. “It tells me that Duke has a culture that attracts a tier of competency at the highest level that is exceptional.”