Fine-tuning Treatments for Breast Cancer
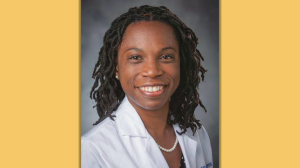
National cancer databases provide a ton of valuable information for researchers, but institutional data is often more granular, including details such as specific chemotherapy regimens, radiation doses, treatment durations, and recurrence rates. The Duke Breast Database (DB2), a big data initiative, is invaluable for health researchers like Oluwadamilola “Lola” Fayanju, MD, assistant professor of surgery and the principal investigator for the database.
“This volume, detail, and quality of data allow us to look at diversity of race, ethnicity, family history, socioeconomic status, and other factors that exist amongst Duke patients so we can better identify population-level trends in breast cancer treatment outcomes,” Fayanju says. “We can even use big data to explore questions that extend outside the medical context, like: How does child care availability or access to transportation affect patients’ ability to get the care they need?”
That’s important information for Fayanju, a breast cancer surgeon whose research is aimed at improving the efficacy and equity with which breast cancer care is provided.
She is leading an analysis of patient-reported outcomes on the Distress Thermometer and Problem List, an ultra-short patient-reported outcome measure that is published by the National Comprehensive Cancer Network (NCCN) and used internationally, including at Duke Cancer Center, and completed at nearly every visit over the course of treatment. The results are entered into the patient’s electronic health record.
“We are using data from 13,000 Duke Cancer Center visits by women diagnosed with breast cancer over 2.5 years to compare distress scores immediately after diagnosis, as well as longitudinally over the course of treatment,” says Fayanju. “Our goal is to use this data to determine whether there are patient, disease, and/or treatment characteristics that are associated with higher or lower levels of reported distress. The hope is that, by identifying these characteristics, we can better inform and advise patients about which treatments are best for them, improve shared decision-making, and better identify potentially vulnerable populations by identifying this data en masse in a way that’s never been looked at before.”
This story was originally published in the Spring 2019 issue of DukeMed Alumni News
Read more about Big Data in Action